|
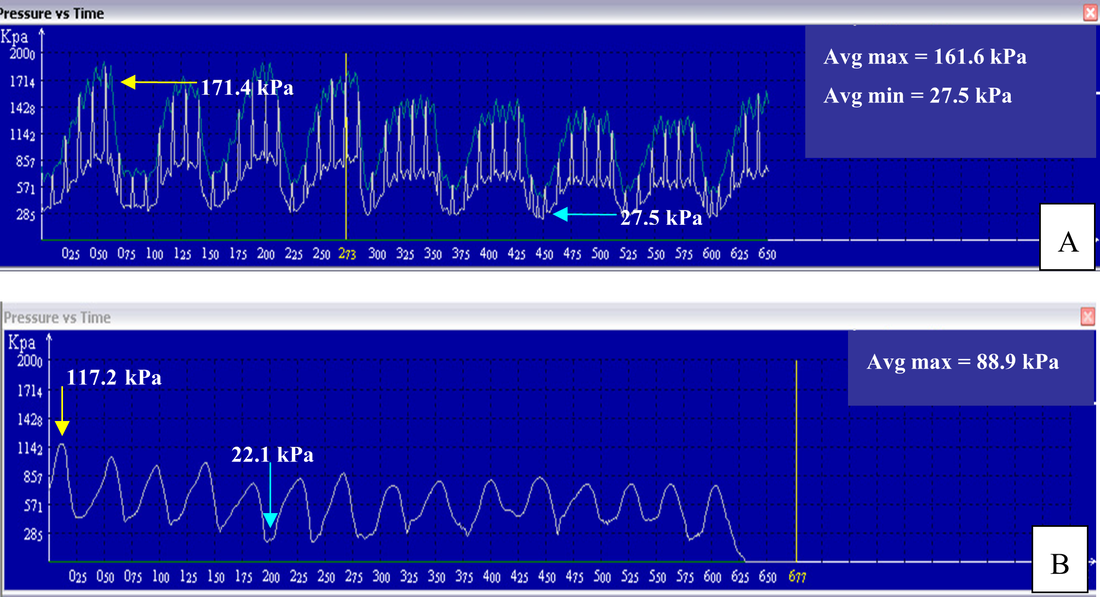
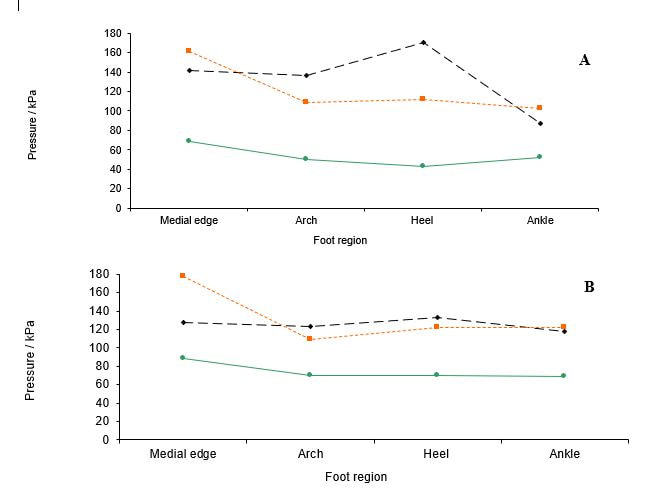
Many of you will know that reflexology uses an applied pressure to initiate a reflex response, and we postulate that it does this via mechanosensitive receptors in the skin. Maybe you learnt that in order to have an effect on an organ or create a physiological response you had to apply a pressure of a certain intensity, but is that true? There is no evidence that tells us what amount of pressure we must apply, so whilst we may discuss light touch, knuckling, rubbing, thumb walking etc. the pressure we apply is purely subjective. In fact, we probably all change the amount of pressure we use according to the general health, age, and size of the client we are treating. But did you know that the skin surface can affect the pressure needed to effectively gain a physiological response? Or that skin thickness can vary between 1.5 and 4 mm depending on the area of the body? For example, a foot that is calloused requires a much greater pressure than a softer foot. As part of my PhD programme of research I wanted to know if there was any difference in the pressure applied when reviewing a person’s pain threshold and tolerance levels, so I carried out a study using a light pressure and my standard reflexology pressure and compared them against no treatment at all. Despite the different pressures, the results of the study revealed a significant increase in pain threshold (a person’s first pain sensation) from both my standard and light reflexology methods. It also revealed a significant increase in pain tolerance (the maximum level of pain one can tolerate) for my standard reflexology, but NOT for my light reflexology. To try to make sense of this I then went on to evaluate the forces of the pressures with a specific objective to measure three different pressure applications. These were a static pressure as used in Nerve Reflexology, a standard on/off dynamic pressure, and a light on/off dynamic pressure, (caterpillar walking). I obtained the Tactilus® Freeform Sensor System V3.1.27 (2007) from an American company who adapted it to suit the needs of my experiment. I went on to measure the pressure at various regions of the foot which included the medial edge of the bony foot, the arch, the heel, and the ankle. I did this on several different foot types so that I could look at the relationship between skin tone, skin texture, age, and the strength of the reflexology stimulus. The four areas of stimulation during the experimental procedure, a) medial edge, b) arch, c) heel d) ankle Physiological impact of pressure on skin tissueWhen skin is put under pressure it changes its geometric shape to accommodate deformation through the displacement of fluid and then returns to its original shape due to elastin in the fibres. Reflexologists are made aware that pressure on the foot sole can have an effect on blood and lymph via the circulatory system and it is the slowly adapting C-fibres of the nervous system that have been identified as being the chief responders in these vasodilatory mechanisms. It doesn’t take much to appreciate that an increased standing or static pressure can intensify the number of callouses in the heel and metatarsal regions. However, this can make it more difficult to effectively stimulate the underlying mechanoreceptors that effect such changes in circulation. My research indicated that using light touch in reflexology can impact pain threshold levels, as well as reducing stress and anxiety, but there is also evidence that static pressure may reduce tension in the paraspinal muscles via a rapid response directly on a nerve or nerve structure. The study I carried out was small with just nine people from a variety of ages (3-79 years), genders and ethnic groups. The different foot types included: normal adult (healthy tone and texture), calloused, moist, soft and spongy, child, oedematous, and hard (dry). What did the results show? As they are considered direct opposites my results focused on pressure applied to both normal and calloused feet. Physiologically there is very little subcutaneous tissue in the medial edge of the foot and the bony skeleton is of course much closer to the surface. What’s interesting about this is that under mechanical load, bone is able to dissipate energy more readily, which implies that pressure may need to be greater on bone in order to achieve a physiological response. The data from my research demonstrated differences of around 50% between my standard and light dynamic pressures (Figures C and D). What was interesting from the research though was that pressure applied to a normal healthy foot is clearly performed in a very precise load/unload pattern with small intermittent steps, (Figure A) reflecting the normal precision of the movement introduced by Ingham. However, in a calloused foot the load/unload impression is less precise (Figure B). Figure A shows the typical on/off caterpillar movement of classic reflexology with a maximum loading of 171.4kPa and a minimum loading of 27.5kPa. In Figure B the same movement performed on a calloused foot provides a maximum pressure loading of 117.2kPa and a minimum of 22.1kPa. The average maximum shows a variation of around 50% for the maximal applied pressure between a normal healthy foot and a calloused foot. Maximum average pressure (kPa) for static, dynamic standard pressure (SR) and dynamic light pressure (LR) on a) normal healthy foot and, b) calloused foot. u Static pressure n Standard reflexology dynamic pressure l Light reflexology dynamic pressure. The experiment showed that pressure applied from a static application was greater than either the standard or light dynamic pressure across all foot regions, and represents the highest maximum average values across the entire experiment. This may be why nerve reflexology has a greater impact on a nerve or nerve tissue than does the usual caterpillar walking of classic reflexology, although research in this area has yet to be validated.
Discussion Most reflexology techniques incorporate the use of a two-handed method of application, inasmuch that whilst one hand holds the foot the other hand stimulates it. Whether it is the tactile sensation acting singly or in combination with the stimuli that provoke a reaction in the cell is unclear at present. However, experience indicates that if the comparisons of reflexology stimulation are matched to the literature on impact of pressures on blood circulation, cellular change, and the mechanisms involved in pain, it would be reasonable to assume that reflexology can initiate physiological change, regardless of the pressure applied. Addendum I recently published an article on my Facebook business page ‘Reflexmaster’ about the two Nobel prize winners for Physiology or Medicine, David Julius and Ardem Parapoutian. Their research on the PIEZ02 receptor and its impact on allodynia, (an extreme reaction to a light touch), may well help throw more light on the mechanism of action of reflexology for supporting clients in pain, and is an incredibly exciting area for future studies. The PIEZ02 ion channel is light-touch sensitive and because both tissue injury and inflammation markedly alter touch perception, normally innocuous sensations become intensely painful. If reflexology can emulate the studies carried out by cell biologists to reduce the sensitivity of the PIEZ02 receptor, we may well be able to demonstrate more scientifically the mechanism of action for its benefits on pain. First published in my PhD thesis ‘An investigation into the efficacy of reflexology on acute pain in healthy human subjects’, Carol Samuel, 2011, University of Portsmouth. Dr Carol Samuel PhD, FFHT, HMAR [email protected] www.reflexmaster.co.uk
1 Comment
|
AuthorDr Carol Samuel PhD Archives
October 2021
Categories |
|
© Copyright - Carol Samuel PhD 2018
All rights reserved |


 RSS Feed
RSS Feed